By Chris Spangler
Another 50 percent of the general population will need be vaccinated against COVID-19 before Jefferson County reaches the desired herd immunity, the Fort Atkinson Rotary Club learned Monday.
Speaking to the club during its virtual weekly meeting was Chris Barron, executive director of Population Health & Clinical Services at Fort HealthCare.
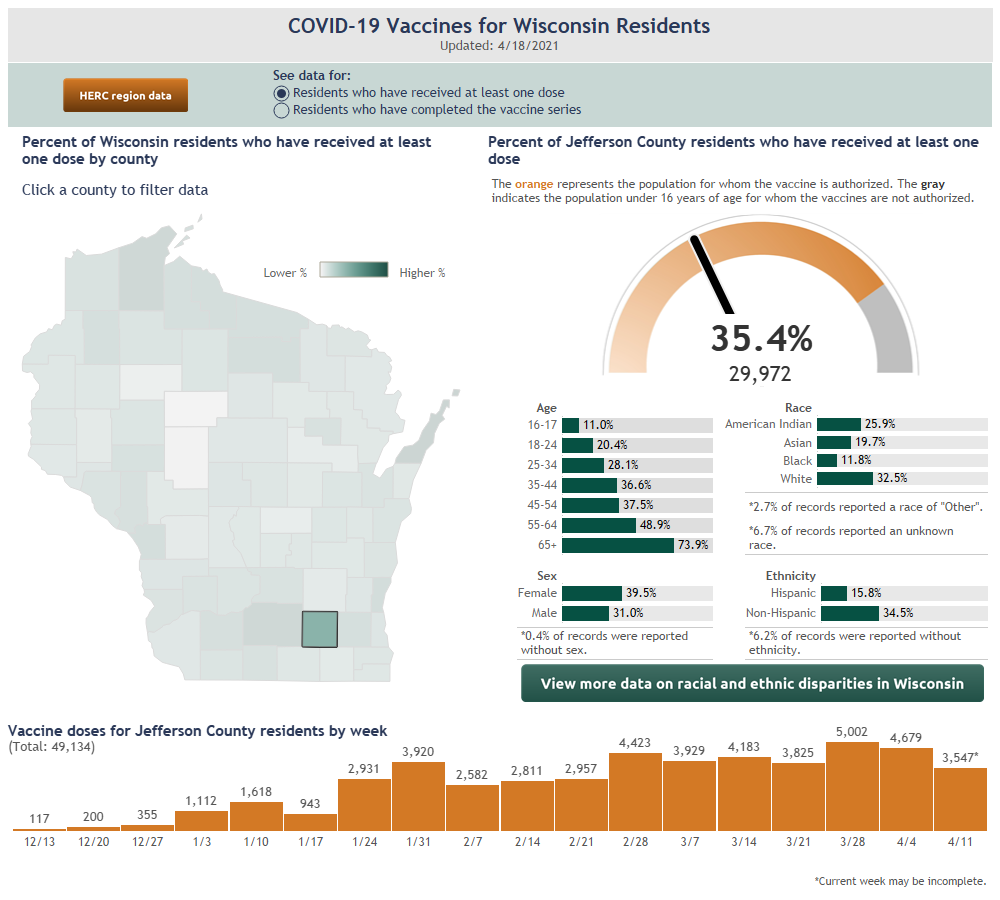
Barron reported that as of Monday, 25.7 percent of county residents had been fully vaccinated against the coronavirus.
“We’re at about a 25-percent vaccination rate for county residents who have completed the series of the vaccine,” he said. “We got a good start; we have a lot of work to do. To get to where we need to be, to achieve some level of herd immunity, we’re about a third of the way to be at about a 75-percent vaccination rate.
“That’s important, because the longer this stays, the more chance there is for variants to take hold,” he added.
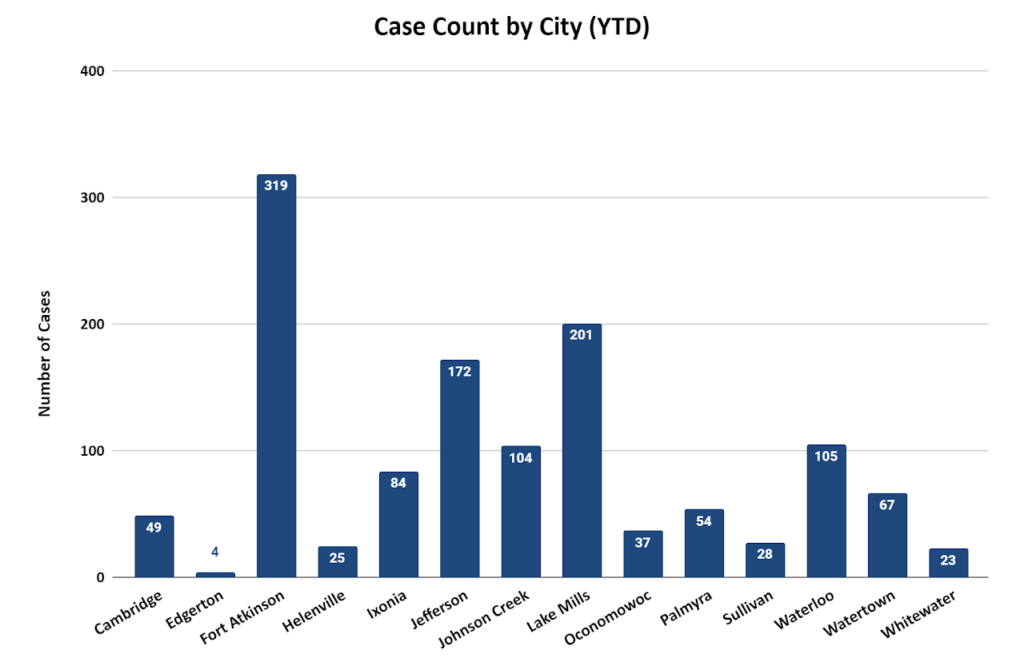
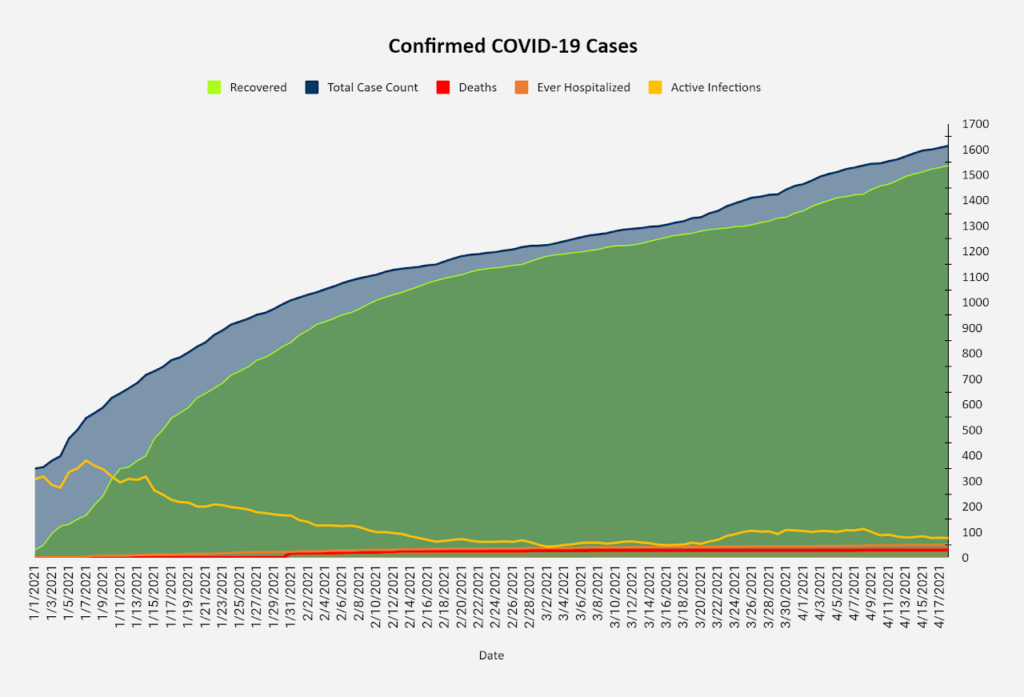
As of Monday, Jefferson County had recorded 8,228 cases of COVID-19, including 319 in Fort Atkinson, and 1,157 probable cases. There have been 108 deaths and another 23 probable deaths due to the coronavirus.
A total 30,157 or 35.6 percent of county residents have received at least one dose of a vaccine, while 21,867 have completed a series.
The largest age group of the latter are those 65 and older, at 68 percent, while the smallest, 16- and 17-year-olds, is at 1.65 percent. Other full vaccination rates are: age 55-64, 28.55 percent; 45-54, 23.5 percent; 35-44, 24 percent; 25-34, 17.9 percent; and 18-24, 11.3 percent.
Barron said that Fort HealthCare has been focusing on connecting with 16- and 17-year-olds so they can get the Pfizer vaccine. The Moderna and Johnson & Johnson vaccines currently are only available for people age 18 and older.
“My hope is that in the months to come, we’ll see a vaccine with the age limit going down and we can open it up,” Barron said of vaccinating children.
That will be important in the trek toward herd immunity.
“To put this into context, we vaccinate for influenza every year.
“In a really good influenza season, we vaccinate about 45 percent of the general population,” he said. “We almost have to double what you do on an annual basis with influenza to get to the level we want to get to with COVID.”
Unfortunately, not everyone is certain they should get vaccinated. Such vaccine hesitancy is something the county vaccine task force talks about weekly because “we have to overcome a lot of vaccine hesitancy to get to the level of vaccination we need to get out of this pandemic,” Barron said, adding that it tries to counter that with facts from reliable sources.
“I think we’ll still have some sectors of the population that will fall on the far (end of the vaccine-hesitant scale),” he said. “Who we want to impact are those folks in the middle that are being influenced one way or another. I think we have a lot of people who, if they get good education, can make good, educated decisions.”
Responding to a question about who pays for vaccinations, Barron said that the federal CARES Act does allow for some reimbursement for administration. However, Fort HealthCare thus far has not sought that reimbursement.
“We did not want to get in the way of us providing care to our community,” he said. “So thus far, we get the vaccines for free, but we’re donating our time and our resources to administer them to people.
“With all the focus on vaccine hesitancy, we certainly don’t want to insert any barriers. We want people to get vaccinated as much as possible.”
Meanwhile, Barron also provided an overview of Fort HealthCare’s COVID-19 response, including ongoing vaccinations, that marked its 411th consecutive day Monday.
“We’ve been at this a long time and will continue at this a little longer,” he told the Rotarians. “We don’t like it either. We would just as well not be dealing with a pandemic, but it is what is in front of us.”
He shared a quote by American motivational writer William Arthur Ward: “The pessimist complains about the wind; the optimist expects it to change; the realist adjusts the sails.”
“We’ve spent the last year adjusting the sails in dealing with what’s in front of us, working with our community partners,” Barron said. “The exercise of pandemic response actually comes down to managing three things: space, staff and stuff.”
That ranges from dealing with how to hospitalize patients in the space, specifically negative air-pressure rooms, to limited personal availability of protective equipment (PPEs), testing supplies and vaccines.
“And then we have to have staff to rise to the occasion to do either pandemic response in the hospital, do testing, give vaccines,” Barron said.
That staff could include not only Fort HealthCare employees, but Jefferson County Health Department personnel, Wisconsin National Guard members, EMTs and other front-line workers.
“We kind of manage that triad throughout the pandemic and usually there’s at least one constraint on one of the corners of the triad,” Barron said. “Sometimes there are two constraints. Sometimes there are three. So we’re always shifting, adjusting and dodging to provide the best care, keep people safe and adjust to the pandemic as we go along.”
He recalled that early on in the pandemic, the hospital had to provide for patients needing isolation and negative-pressure space. But it only had six negative-pressure rooms at the time. Today, Fort Memorial Hospital has expanded that to 16 negative-pressure rooms on the inpatient unit and another one in obstetrics.
“That’s an example of the innovation that’s been going on around here to adjust and actually expand capacity on the space side,” Barron said.
As for staffing, Fort HealthCare wound down some operations to free up resources in anticipation of a surge that was anticipated in spring to summer but didn’t arrive until November and December. At the same time, it was experiencing many of the same pandemic issues as other businesses out in the community.
“Some staff caught COVID-19 in the community and needed to be home, we had staff that were quarantined, we had staff with kids out of school,” Barron explained. “So we had the same workforce issues as other employers throughout the region … We did some creative things to accommodate time off, keep people home when sick.
“To this day, I don’t think we have traced any COVID cases that have been caught at our institution,” he said.
Fort HealthCare also extended a lot of effort in infection prevention, of course.
“I like to stress that we’re experts in infection prevention: this is what we do. If its not COVID, we’re preventing colitis or the spread of other infectious disease within our organization. So we already have processes in place to deal with infectious disease,” Barron emphasized.
“When you think about a hospital like us, we don’t have a hospital just full of sick people,” he continued. “We have well people, too. We have people getting new hips and knees, people delivering babies … We have to keep the well people from getting sick.”
COVID-19 did pose some new challenges, he said, citing the limited PPEs and other supplies, but that was an extension of the infection-prevention practices already in place.
“The other thing unique about COVID is just the scale of it. We might see, during the winter, outbreaks of influenza or pneumonia and things like that, but the sheer scale of this in the community was something that really impacted us,” Barron said.
He noted that during the past 411 days, Fort HealthCare has been working behind the scenes on the local, county, state and national levels. It is involved in the Emergency Operations Center assembled by Jefferson County Administrator Ben Wehmeier, county and state health officials, and “some of the brightest and most determined people I know” at the Centers for Disease Control and Department Health and Human Services.
“A year later, we still do have some supply chain issues,” Barron said, adding that the hospital has adequate PPEs and testing supplies, but he is “continuously a little nervous” about keeping them in stock.
And during the past three to four months, a main concern has been getting enough vaccines.
He said the countywide vaccine task force includes a wonderful group of engaged stakeholders ranging from pharmacies and health systems to health departments and more is being led by the county epidemiologist.
“We now are trying to solve this puzzle of providing vaccines adequately and equitably,” Barron said. “Were committed to working with our partners and address issues such as vaccine hesitancy and equitable access … If you can get the vaccine, get vaccinated. That is the best thing we can do to slow the spread of COVID.
“It’s not only important to vaccinate the vulnerable populations, but you also have to vaccinate the spreaders,” he added. “This is how communicable diseases work.”
He re-emphasized that there remain large segments of the population that can not be vaccinated yet, such as children under age 16 and persons in certain risk groups.
In addition, the Johnson & Johnson vaccine was paused temporarily out of an abundance of caution to study the risk for rare blood clots.
“Likely we’ll see that vaccine coming back on the market with some additional warnings on it for additional risk groups,” Barron said.
As for what’s next, he said that Fort HealthCare simply must continue to vaccinate in an effort to reach herd immunity.
“I think we’ll likely see some version of a booster shot in years to come, as well as we’ll be living with COVID here,” Barron said. “Our staff here at the hospital are resilient, adapting and collaborating. So many thanks to our frontline staff and to everyone in the community working on this issue.
“We’ve been intently focused the past year on dealing with the pandemic. What we’re switching gears to now is to the collateral damage of the pandemic,” Barron added.
“We have patients who have put off care during the past year.”
He cited preventative care, childhood vaccinations and chronic conditions such as diabetes, heart failure and hypertension.
And then there are what he calls diseases of despair: substance abuse, physical abuse and behavioral health issues resulting from the pandemic.
“There will be a lot of work on things like that into the future,” Barron concluded.
Educated at the University of Wisconsin-Madison and the Academy of Health Sciences in Fort Sam Houston, Texas, Barron has worked in the health system pharmacy field for more than 20 years. His work as a pharmacist has found him in roles ranging from clinical and critical care pharmacist to clinical pharmacy coordinator, medical informatics and as pharmacy director.
In 2015, Barron left the pharmacy to take his current position overseeing Fort HealthCare’s internal and external population health initiatives. He uses data and analytics to measure outcomes in order to foster improvement in those outcomes.

Chris Barron
This post has already been read 1105 times!