By Kim McDarison
The Whitewater Common Council Tuesday discussed bringing a referendum before voters to fund, in part, an increase in emergency medical services (EMS) staffing.
If approved by council, a referendum question would likely appear on the ballot in November, Whitewater City Manager Cameron Clapper said.
Details about proposed upgrades to the city’s EMS, changes within the city’s fire department, and plans to fit the two divisions together, as well as details about the overall cost of the proposals and from where funding might come were still in the development stages, and would come before council as the steps developed, Clapper said.
During the meeting, council members received a presentation given by Whitewater EMS Chief Ashley Vickers and Dr. Steven Andrews, an EMS physician with Aurora medical centers. Andrews was introduced to council by Clapper as Whitewater’s medical director for EMS. Responding to questions, Andrews said, along with Whitewater, he serves 17 other EMS departments in a similar capacity.
Aided by slides, Vickers shared some EMS statistics and a proposal to increase staffing within the city’s EMS division by hiring five full-time paramedics.
EMS staffing and call volume
Vickers began the presentation by sharing information about the staffing and operations of the city’s EMS division.
The EMS membership responds to 911 calls for service, in full or in part, within the city of Whitewater and towns of Whitewater, Cold Spring, Richmond, Lima and Koshkonong, Vickers said.
The EMS department has 40 members, six of whom are paid on call and respond from home. The remaining 34 are paid on premise and respond from the station, she noted.
At its current staffing level, Vickers said, the EMS division has two full-time Advanced Emergency Medical Technicians (AEMTs) and three full-time Emergency Medical Technicians (EMTs), whom, she said, are scheduled during daytime hours, Monday through Friday.
Additionally, the department has five paramedics, 17 AEMTs and 16 EMTs.
Looking at call volume, Vickers said, in 2021, the EMS division received 1,620 calls for ambulance service. Of those calls, 272 were “second calls,” meaning a first ambulance and its crew were already on a call when those calls came in. Additionally, the division received 22 “third calls” and one “fourth call.”
In 2022, Vickers said, the division has received 147 total calls, with 28 of those resulting in a need for a second ambulance, eight calls resulting in a need for a third ambulance and two resulting in a need for a fourth ambulance.
In response to those calls, mutual aid was requested twice, with both of those requests coming in response to a second call for ambulance service, she said.
The average response time in 2022 has been 3.66 minutes, Vickers reported.
In Whitewater, she said, the division’s first ambulance is staffed with an AEMT and an EMT. Two full-time EMTs work Monday through Friday, from 6 a.m. to 6 p.m.
A second ambulance is staffed with two EMTs with an emphasis placed on those crew members who have both EMT and firefighting skills. The crew is cross-staffed for both the ambulance and an engine, according to a slide shared by Vickers.
EMS members, with the exception of two paid-on-premise AEMTs, work monthly 12-hour mandatory shifts which are scheduled by the assistant chief of the EMS Division. The shifts cover Fridays at 8 p.m. to Sundays at 8 p.m., information on a slide indicated.
The current EMS hourly pay structure is as follows: AEMT, full-time, paid on premise, $22; flex AEMT, paid on premise, $19; EMT, full-time, paid on premise, $18; AEMT, paid on call (respond from home), $17; second ambulance, firefighter/EMT, $13; EMT, paid on call, $14; EMT, paid on premise, $16; second ambulance, EMT, $12, and trainee, $7.25.
Proposed paramedic upgrade
Under the heading of “Proposed Paramedic Upgrade,” Vickers outlined the following: the department would continue to staff the first and second responding ambulances with two EMTs or AEMTs, or a two-man crew with members at each of those training levels.
In addition to the department’s existing membership, the department would hire five full-time paramedics at a starting hourly wage of $25, and the new hires would receive benefits.
When responding to calls, paramedics would respond in a “chase vehicle” to all first calls and perform an advanced life support (ALS) level assessment, which would determine if that level of care was needed for the safe transport of the patient. If an ALS level was required, the paramedics would make the transport. If not, the paramedics would return to the station to receive incoming calls and two EMTs would transport the patient as a basic life support (BLS) level call.
Sharing a slide titled: “Previously approved plan,” Vickers noted, “This plan is the same as previously approved, but at the paramedic level instead of the AEMT level.”
The plan, a council member noted in a followup comment on Friday, was previously approved by the Whitewater Fire Department, Inc., Board of Directors.
Within the presentation, Vickers cited high call volume and high acuity calls (defined as calls meeting trauma triage criteria for treatment or receiving treatment for acute conditions such as coronary syndrome, respiratory distress, altered mental status, acute stroke, allergic reaction or abnormal vital signs) as reasons for a need for a paramedic-level quality of care in Whitewater.
Wait times for paramedics to respond from other jurisdictions such as Jefferson or Janesville cost valuable time, Vickers said, noting that in the field of EMS, an expression used is “time is tissue,” meaning life depends on a quick response.
Comparing the differences between AEMT and paramedic-level skills, Vickers said, among procedures a paramedic can perform that an AEMT cannot, are: advanced airway interventions; electrical interventions for cardiac arrhythmias, and administering medications used to stop seizures, control heart rhythms, control blood pressure, pain, and stop nausea and vomiting.
Further, a slide stated: “paramedics have also been shown to have a relative reduction in mortality compared to the current AEMT level of service in several different conditions,” including, reducing death from heart attacks by 47%, reducing death from all causes of chest pain by 45%, and reducing death from respiratory distress by 13%.
Vickers next shared wages as paid to paramedics serving in area departments including the Jefferson Fire Department, where paramedics receive hourly wages between $24 and $26, and the Edgerton Fire Department, where paramedics receive hourly wages of approximately $24.
Costs
Looking at budgets and costs, Vickers said in 2021, the budget anticipated to cover the cost of EMS staffing in Whitewater was set at $296,838. The actual amount spent was $287,191.
A slide shared by Vickers showed a previously approved AEMT-level staffing budget of $641,680, which, the slide indicated, was an increase of $344,842 over the budgeted amount in 2021.
Sharing a slide with costs associated with the proposed paramedic upgrade, Vickers said the staffing provision would require a budget of $801,528, which would bring an increase of $504,690 as compared with dollars budgeted for EMS staffing in 2021.
As part of the presentation, a slide shared increased ambulance rates for 2022, noting that the increased rates could bring an “increase in revenue for 2022 by approximately $118,000 at the AEMT level,” and an “increase in revenue at the paramedic level (that) would equate to approximately an additional $100,000 annually.”
‘How do we pay for this?’
After the presentation, Clapper opened discussion with a question. He asked: “How do we pay for this?”
He noted that the EMS proposal was driven by “a need to catch up our emergency medical service to what our community actually is in need of and what many of our community members already think they are getting.”
To achieve that goal, Clapper said, council had two options.
“One is we don’t change anything about our tax levy and as a result we make dramatic changes and shifts to every other service that we provide to accommodate changes with EMS.”
Or, he said, “We pursue a referendum and address the funding gap by way of that referendum in November.”
Earlier Tuesday, Clapper said, city staff held a meeting to become familiar with scheduling requirements associated with bringing a referendum forward.
In terms of funding options, he said, “right now, it’s magic money … that’s a joke; I don’t know if it’s funny or not.”
He said city staff was looking at fund balances to see how they might be applied.
A council member asked if the city’s demographics were contributing to elevated call volumes.
Vickers responded, saying: “I would say a good majority of our calls is a geriatric population … We do visit the assisted living facilities, the nursing homes, we go to those quite a bit. We do also tend to frequent the lower income housing and the group homes as well.”
Looking at possible strategies to reduce call volume, Clapper said: “I can tell you that I do believe that there are ways for us, in some ordinances and other means, to assist in shifting the burden to the actual care facility rather than allowing them or letting them take advantage of our EMS program, our fire department’s EMTs. Some of that’s been done, but I think there’s probably more things we can do; I just haven’t explored it yet.”
Said Vickers: “We’ve implemented some things internally, such as … when we see frequent fliers for routine things, especially like lift assists, you know, somebody that’s not injured, but they just need assistance up. So we give them one freebie, but if they call us multiple times within a certain time period, we start billing them.”
Vickers added: “Working with the Walworth County crisis worker has helped tremendously with some of the frequent fliers that we’ve had. Especially with mental health concerns or substance issues, so that has been a big help for us.”
Returning to the question of options and the EMS paramedic upgrade, Clapper said: “So tonight, the council has a few options. I think one important one is making sure you all have heard about it and became aware of it. The fire department board of directors has approved moving forward with it subject to any actions taken by the council. We could act tonight to say, ‘yeah, let’s do it,’ or you could act tonight to say, ‘let’s get all the kinks worked out so we can pull the trigger on it right after the referendum,’ or anything in between there.”
In an ideal set of circumstances, Clapper said, “I think … we say, yes, and then we get started on moving forward, but I do have to caution … we’ve committed to the fire department that we are supportive of their plan, and we acknowledge the need to staff,” but, he added, “The budget that was approved recognizes funding at a level that is now obsolete, with the understanding that we would need to do a referendum or significantly change other services by year end 2022.”
Looking ahead, Clapper said, next steps would include informing the public and “identifying the parameters of the whole,” asking: “What does that egg look like? How big is it? And then being able to take time and go through all the details of what comprises that egg, and then getting that information out into the community early in this summer most likely.”
Referencing numbers presented by Vickers, Whitewater Finance and Administrative Services Director Steve Hatton said: “I’ve received this for the first time today, so I need to work with Ashley go through it. This is the EMS piece of it, for the ambulance, but to put that into the entire fire and EMS budget and compare where we budgeted and approved for ’22 versus what this would entail and the full picture, that work needs to be done.”
“My guess is this body would be very favorable towards having paramedics. It’s a matter of paying for it. Also, I would suspect it’s a matter of how feasible it is to even hire them — paramedics — in this area. I really wonder if ultimately you might end up finding that we might need to grow some paramedics from within our own existing staff,” Council President Lynn Binnie said.
Addressing questions about a timeline, Vickers said: “It’s going to take some time to not only outfit our current ambulances to the paramedic level, but also acquire all the medications, supplies, and then submitting the operational plan to the state, which, the state is not very quick on turn-around times, so, I mean, realistically, if we said tomorrow that we can go ahead with it, it would probably be summer before we’d even have it operational.”

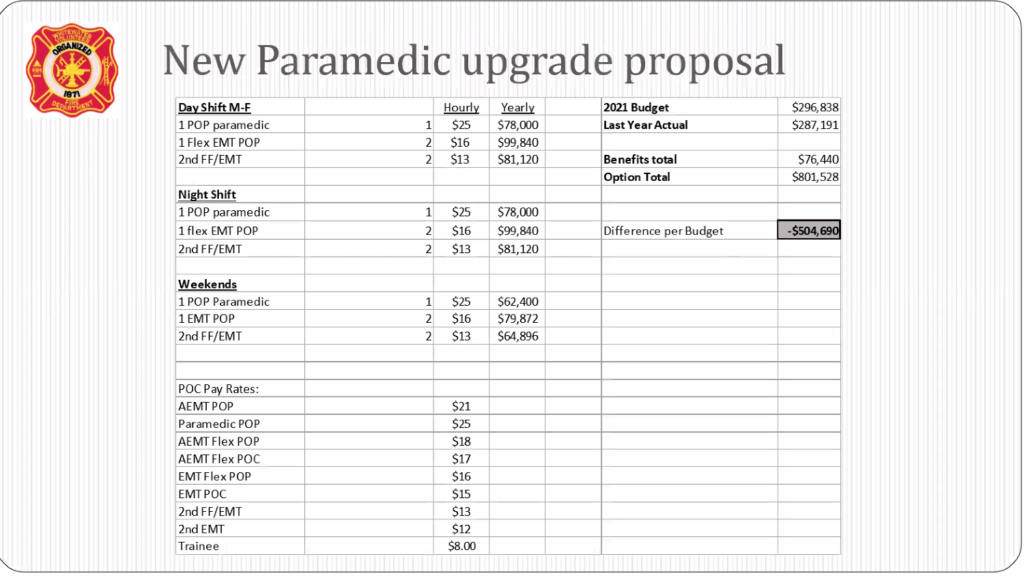
Two graphics above as supplied by Whitewater EMS Chief Ashley Vickers shows budgeted costs associated with EMS in 2021, as well as budgeted amounts associated with an approved proposal to increase staff with full-time AEMTs and upgrading to increasing staff with full-time paramedics. The proposal to increase staff with AEMTs was approved by the Whitewater Fire Department, Inc., Board of Directors.

Whitewater EMS Chief Ashley Vickers, from left, and Dr. Steven Andrews, an EMS physician with Aurora medical centers who serves as Whitewater’s medical director for EMS, address the Whitewater Common Council Tuesday. The EMS professionals shared with council a proposal to increase the Whitewater EMS division staff by five full-time paramedics.
Update: This story has been updated to include comments shared Friday by a council member indicating that the EMT plan presented Tuesday as “previously approved” was approved by the Whitewater Fire Department Inc., Board of Directors.
This post has already been read 1826 times!
